Hyperosmolar Nonketotic Coma: Clinical Significance, Diagnosis, Treatment, Course And Prognosis
Hyperosmolar Nonketotic Coma

A General Overview And Diagnosis
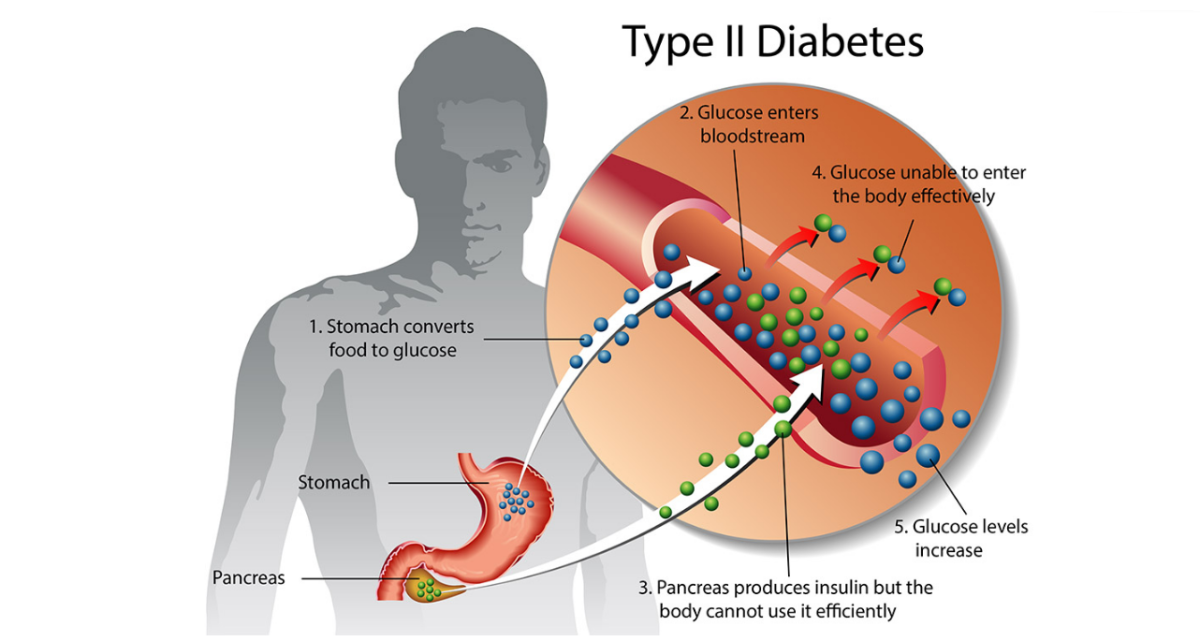
This is a serious emergency, seen occasionally in elderly diabetics. The condition is precipitated by infection, myocardial infarction, burns, trauma, surgical stress, renal failure, pancreatitis and the use of certain drugs like thiazide diuretics, steroids and propranolol. In this condition, probably a small amount of endogenous insulin is present so that lipolysis does not occur, but glucose metabolism is grossly deranged. Blood sugar level often exceeds 600 mg/dl. Ketoacidosis is absent and this distinguishes the condition from diabetic coma.
Plasma osmolarity rises above 360 mosmol/liter and there is profound cellular dehydration. The hematocrit is high. When the fluid loss becomes severe, hypernatremia develops. Sodium ions are critically important in determining plasma osmolarity. Body potassium is lost and a total deficit of 40 to 100 meq may occur.
The normal plasma osmolarity ranges from 280 to 310 mosmol/liter. Values above 340 mosmol/liter are abnormal. In severe cases, the osmolarity may exceed 370 mosmol/liter. The condition starts with extreme weakness and drowsiness and the patient slips into coma. Other neurological manifestations such as seizures, ataxia, hemiparesis, aphasiz and mental disturbances may be present. Though, thirst is present in the early stages, it disappears later. Respiration is normal or depressed. Apart from these fractures, the picture may resemble that of diabetic coma.
Diagnosis
Hyperosmolar nonketotic coma should be suspected in all cases of coma occurring in diabetics, without demonstrable ketosis. Plasma osmolarity can be calculated from the plasma levels of sodium, potassium, glucose, and urea using some formula.
Treatment Of Hyperosmolar NonKetonic Coma

Treatment
Principles of management include correction of the extreme depletion and hyperosmolar state. Insulin is administered in small doses as soon are preferable since these patients are very sensitive to even small doses of 10 to 20 units intravenously, every two hours till the blood sugar falls to 200 mg/dl. Alternatively, 20 units of soluble insulin may be given intramuscularly, followed by small disease of 5 to 10 units every hour.
Hypotonic fluids are administered to lower the osmolarity. Half normal saline is the fluid of choice. About 6 to 8 liters may have to be given over 24 hours. Monitoring of central venous pressure is essential in the elderly to avoid fluid overloading and cardiac failure. In pateitns with shock, isotonic saline should be infused till the central venous pressure begins to rise.
Potassium should be replaced early during the treatment and it should be monitored with serum potassium estimations. The total deficit may be as high as 200 to 300 mEq/liter.
Course and prognosis: The prognosis is grave and mortality may be 20 to 40%. Prompt and early treatment results in recovery.
© 2014 Funom Theophilus Makama