Clinical Manifestations Of Lobar Pneumonia And Extrapulmonary Pneumococcal Lesions
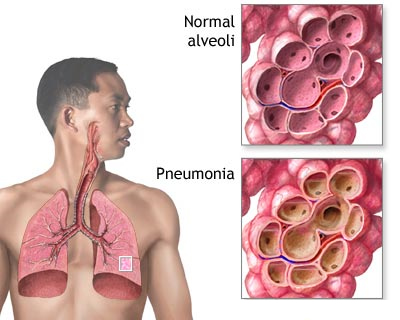
A Pneumonia Patient

Clinical Manifestations
Pneumonia is often preceded by coryzea or other upper respiratory tract infections. Incidence of pneumonia is higher in males. The onset is sudden with fever and chills in the majority of cases. There is marked tachycardia and tachypnea. The alaenasi are seen to move when the patient breathes. Severe pleuritic pain and cough with expectoration of pinkish or rusty mucoid sputum follows. The respiration becomes rapid and shallow and may be associated with grunting. Respiratory embarrassment results in cyanosis. The patient becomes very ill and toxic. In the untreated case, fever persists continuously for 7 to 11 days after which it comes down by crisis. It is common to get a crop of labial herpes simplex during the fever.
Physical examination reveals rapid pulse, fever and signs of consolidation over the affected lobe of the lung. As resolution starts, coarse crepitations develop. If pleurisy occurs, pleural friction rub may be elicitable. In uncomplicated cases, once the temperature comes down, the patient feels well and recovery starts. However, the pulmonary lesions resolve completely only after a few weeks.
Early institution of specific therapy can prevent the development of consolidation and the general symptoms, but if consolidation has been established, resolution takes time, depending on the body’s netural defences. The response to penicillin therapy is dramatic.
Laboratory findings: Sputum is rusty in colour. Pneumococci can be demonstrated by Gram staining. Blood culture is positive in 20 to 25% of cases in the early stage of the disease. There is marked leucocytosis ranging from 12,000 to 25,000 cells/cu.mm and neutrophils from 85 to 90% of the total. Absence of leucocytosis or even leucopenia may sometimes be observed in patients with overwhelming infection and bacteremia. The prognosis in such cases is very poor. Skiagram of the chest shows a homogenous opacity corresponding to the lobe involved.
Complications: Local complications include atelectasis, lung abscess and delayed resolution. Spread of inflammation to adjacent structures leads to pleural effusion, empyem, pericarditis and peritonitis. Hematogenous spread results in septicemia, meningitis, and acute endocarditis. Gastrointestinal complications include paralytic ileus, gastric dilatation, impairment of liver function and jaundice.
Prognosis: Is the vast majority of cases the lesion subsides and recovery is complete. Adverse prognostic signs include leucopenia, bacteremia, mutilobar involvement, extrapulmonary involvement, circulatory collapse, presence of pre-existing systemic diseases and occurrence of the disease at the two extremes of life (below 3 years and above 55 years). Infection with type 3 pneumococcus has a higher mortality rate.
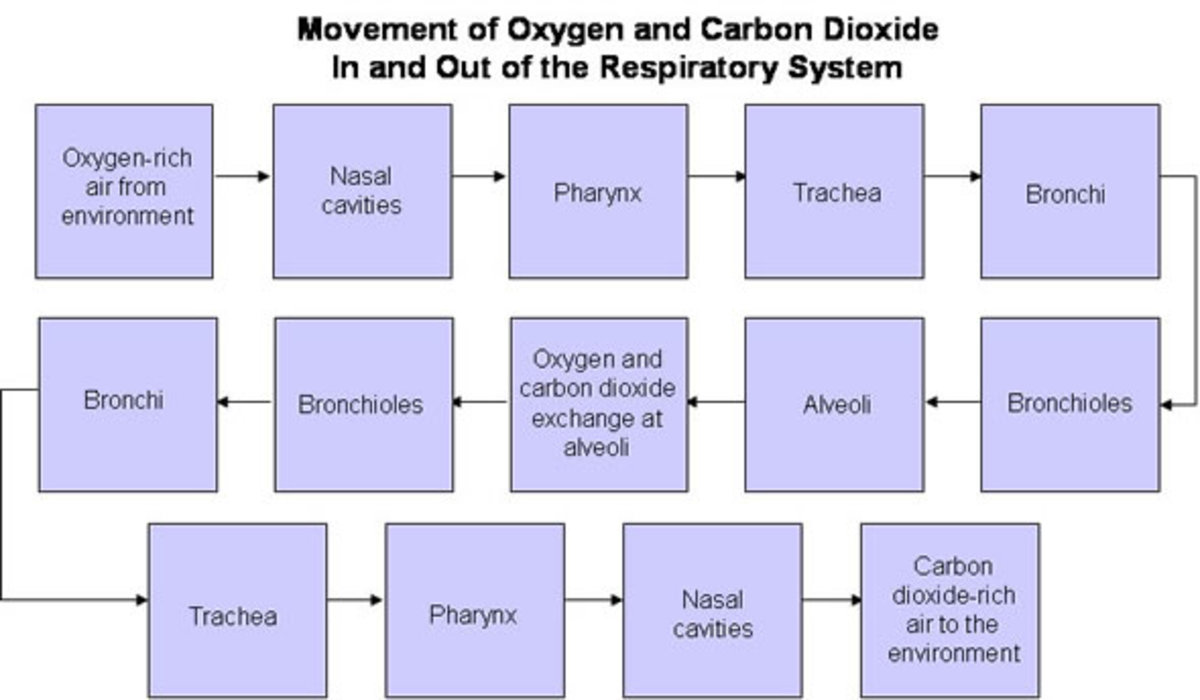
How Pneumonia Is Manifested
Extrapulmonary Pneumococcal Lesions
Pneumococcal meningitis: Pneumococcal meningitis may develop primarily or this may be a complication of pneumococcal pneumonia, otitis media, mastoiditis or sinusitis.
Pneumococcal peritonitis: This is a rare infection. It is more frequent in girls, patients with nephrotic syndrome, cirrhosis of liver and abdominal malignancies.
Treatment of pneumococcal infections: Pneumococci are generally susceptible to penicillin, but resistant strains are being reported. It is advisable to send the sputum for sensitivity tests before starting specific therapy. Benzyl penicillin is the drug of choice for pneumococcal infections.
Pneumonia: Crystalline penicillin is given intramuscularly in a dose of 0.5 mega units/ 8 hours till the temperature comes down to normal and then procaine penicillin in a dose of 0.5 to 1 mega unit daily is substituted and continued till the patient is well on the road to recovery. In the ordinary case, the antibiotic has to be administered for a total duration of 7 to 10 days. When resolution is delayed, the cause should be detected by investigations. An alternative to penicillin is ampicillin, 250 mg 6 hours for 7 to 10 days.
The abnormal physical findings in the chest clear in 2 to 3 weeks. The skiagram may show abnormalities for up to 2 weeks after the temperature comes down to normal. Delay in resolution is due to bronchial obstruction or other underlying lung diseases. Multiple- drug resistant pneumococci respond to vancomycin, 2g/day in divided doses.
Symptomatic treatment includes analgesics (aspirin) for chest pain, oxygen, inhalation, non-narcotic sedatives (diazepam) and expectorants for clearing the respiratory passages. Medicated steam inhalations such as tincture benzoin co or eucalyptus oil provide symptomatic relief and assist expectoration. It is important to ensure adequate convalescence ( at least 2 weeks) after lobar pneumonia and this helps in reducing the sequelae.
© 2014 Funom Theophilus Makama